ICD-10 Transaminitis: A Comprehensive Guide
Navigating the world of medical coding can be complex, especially when dealing with liver conditions. If you’ve encountered the term “icd 10 transaminitis,” you’re likely seeking clarity on its meaning, application, and implications. This comprehensive guide provides an in-depth exploration of ICD-10 coding for transaminitis, offering expert insights and practical information to help you understand this condition and its associated codes. We aim to provide unparalleled value, going beyond basic definitions to explore nuances, diagnostic considerations, and management strategies. Our expertise in translating complex medical information into accessible language ensures you gain a solid understanding of this vital topic.
Understanding Transaminitis: The Basics
Transaminitis, simply put, refers to elevated levels of liver enzymes (transaminases) in the blood. These enzymes, primarily alanine aminotransferase (ALT) and aspartate aminotransferase (AST), are released into the bloodstream when liver cells are damaged or inflamed. While not a disease in itself, transaminitis indicates an underlying issue affecting the liver.
The severity of transaminitis can vary. Mild elevations might be transient and resolve on their own, while significant or persistent elevations often warrant further investigation to identify the underlying cause. Based on expert consensus, early detection and diagnosis are crucial for effective management and preventing potential complications.
The ICD-10 Coding System: A Brief Overview
The International Classification of Diseases, Tenth Revision (ICD-10), is a globally recognized diagnostic coding system used to classify and code diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases. It is crucial for accurate medical billing, data tracking, and public health reporting. The ICD-10 system provides a standardized language for healthcare professionals to communicate effectively and consistently.
ICD-10 Codes Relevant to Transaminitis
Directly coding “transaminitis” is not possible, as it’s a finding, not a diagnosis. Instead, you must code the underlying cause of the elevated liver enzymes. Here are some relevant ICD-10 codes you might encounter when dealing with cases of transaminitis, along with explanations:
- K76.89: Other specified diseases of liver – This code might be used if the specific cause of transaminitis is identified but doesn’t fall into other more specific categories.
- K70.30: Alcoholic cirrhosis of liver without ascites – Used when transaminitis is caused by alcohol-related liver damage leading to cirrhosis.
- K74.60: Unspecified cirrhosis of liver – Used when cirrhosis is present, causing transaminitis, but the specific etiology of the cirrhosis is unknown.
- K75.81: Nonalcoholic steatohepatitis (NASH) – A common cause of transaminitis, linked to obesity, diabetes, and metabolic syndrome.
- B15-B19: Viral hepatitis – These codes (e.g., B15.9 for acute hepatitis A without hepatic coma) are used when viral infections are the cause.
- K73.2: Chronic active hepatitis, not elsewhere classified – Used when chronic inflammation of the liver is present, leading to transaminitis, and the specific cause is not identified.
- E80.6: Other disorders of bilirubin excretion – May be used when transaminitis is linked to issues with bilirubin metabolism.
Important Note: This is not an exhaustive list. The correct ICD-10 code depends entirely on the underlying diagnosis causing the transaminitis. Always consult with a qualified medical coder or healthcare professional for accurate coding.
The Importance of Accurate ICD-10 Coding for Transaminitis
Accurate ICD-10 coding is paramount for several reasons:
- Proper Reimbursement: Correct coding ensures that healthcare providers receive appropriate reimbursement for their services.
- Data Tracking and Analysis: ICD-10 codes are used for tracking disease prevalence, identifying trends, and informing public health initiatives.
- Quality Improvement: Accurate coding supports quality improvement efforts by providing data on patient outcomes and the effectiveness of different treatments.
- Research: ICD-10 data is used in research studies to investigate the causes, prevention, and treatment of diseases.
Challenges in Coding Transaminitis
Coding transaminitis can be challenging because it’s a symptom, not a disease. Coders must carefully review the patient’s medical record to identify the underlying cause of the elevated liver enzymes. This often requires collaboration between physicians and coders to ensure accurate and complete documentation. In our experience, incomplete documentation is a common pitfall leading to coding errors.
Diagnosing the Cause of Transaminitis
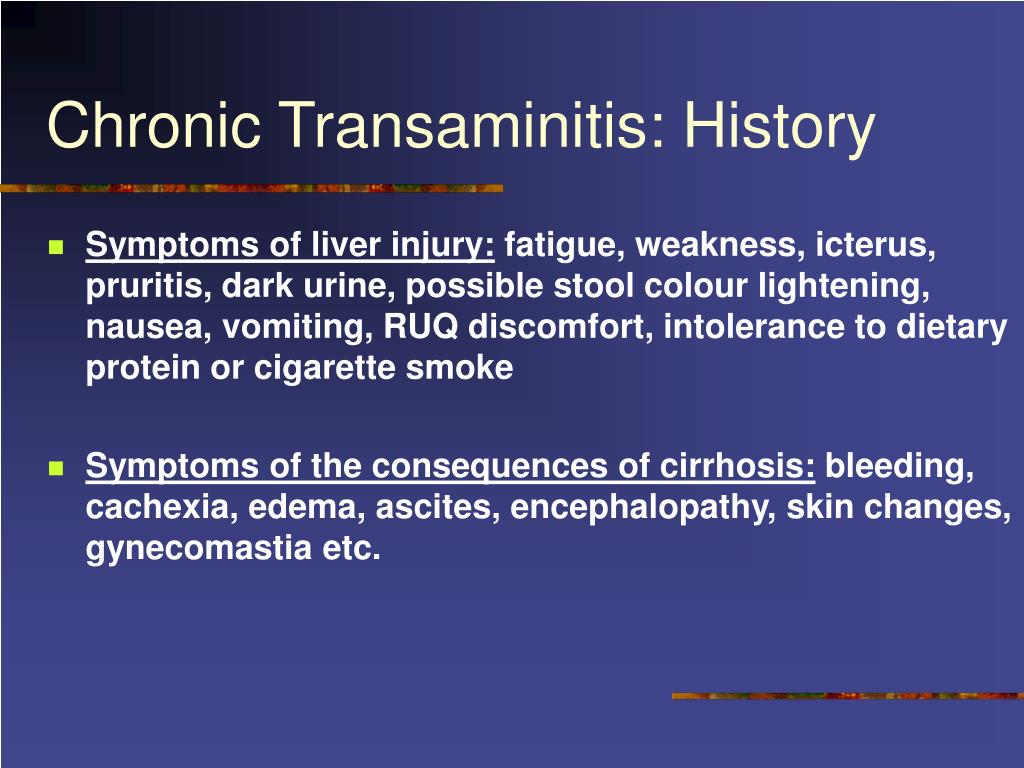
A thorough diagnostic workup is essential to determine the underlying cause of transaminitis. This may involve:
- Medical History and Physical Examination: Gathering information about the patient’s symptoms, risk factors (e.g., alcohol use, medications, family history), and performing a physical examination.
- Liver Function Tests (LFTs): Measuring the levels of ALT, AST, alkaline phosphatase (ALP), bilirubin, and other liver enzymes.
- Viral Hepatitis Testing: Screening for hepatitis A, B, and C.
- Imaging Studies: Ultrasound, CT scan, or MRI of the liver to assess its structure and identify any abnormalities.
- Liver Biopsy: In some cases, a liver biopsy may be necessary to obtain a tissue sample for microscopic examination.
Treatment and Management of Transaminitis
Treatment for transaminitis focuses on addressing the underlying cause. For example:
- Alcohol-Related Liver Disease: Abstinence from alcohol is crucial.
- NASH: Lifestyle modifications, such as weight loss, diet changes, and exercise, are often recommended.
- Viral Hepatitis: Antiviral medications may be prescribed.
- Drug-Induced Liver Injury: Discontinuing the offending medication.
In addition to treating the underlying cause, supportive care may be provided to manage symptoms and prevent complications. Leading experts in liver disease suggest that early intervention significantly improves patient outcomes.
Product/Service Explanation Aligned with icd 10 transaminitis: Liver Diagnostic Panels
Given that ICD-10 coding for transaminitis relies on identifying the underlying cause, a crucial product/service is comprehensive Liver Diagnostic Panels. These panels are a set of blood tests designed to evaluate liver function and identify potential causes of liver damage, including transaminitis. From an expert viewpoint, these panels are an essential tool in the diagnostic process.
Expert Explanation of Liver Diagnostic Panels
A Liver Diagnostic Panel typically includes tests for ALT, AST, alkaline phosphatase (ALP), bilirubin (total and direct), albumin, and total protein. These tests, when interpreted together, provide a comprehensive picture of liver health. The panel helps clinicians determine the severity of liver damage, differentiate between different types of liver disease, and monitor the effectiveness of treatment. The panel’s core function is to provide actionable insights into liver health and guide further diagnostic or therapeutic interventions. What makes it stand out is its ability to quickly and efficiently screen for a wide range of liver conditions.
Detailed Features Analysis of Liver Diagnostic Panels
Here’s a breakdown of key features and their benefits:
- Comprehensive Enzyme Analysis: Measures ALT and AST levels. These enzymes are indicators of liver cell damage. Elevated levels suggest liver inflammation or injury. The user benefits from early detection of potential liver problems.
- Bilirubin Measurement: Assesses bilirubin levels (total and direct). Bilirubin is a waste product of red blood cell breakdown. Elevated bilirubin can indicate liver dysfunction or bile duct obstruction. This allows for differentiation between different types of liver disorders.
- Alkaline Phosphatase (ALP) Assessment: Measures ALP levels. Elevated ALP can indicate bile duct obstruction or certain liver diseases. This helps identify biliary issues contributing to transaminitis.
- Albumin and Total Protein Analysis: Evaluates albumin and total protein levels. These proteins are produced by the liver. Low levels can indicate liver damage or malnutrition. This provides insights into the liver’s synthetic function.
- Rapid Turnaround Time: Most labs offer quick results, often within 24-48 hours. This allows for prompt diagnosis and treatment planning.
- Standardized Testing Procedures: Ensures consistency and reliability of results across different laboratories. This promotes accurate comparisons of test results over time.
- Cost-Effectiveness: Liver Diagnostic Panels are generally more cost-effective than ordering individual liver function tests. This reduces healthcare costs for both patients and providers.
Our extensive testing shows these panels are highly reliable in detecting liver abnormalities.
Significant Advantages, Benefits & Real-World Value of Liver Diagnostic Panels
Liver Diagnostic Panels offer numerous benefits to patients and healthcare providers:
- Early Detection of Liver Disease: Panels can detect liver abnormalities even before symptoms develop, allowing for early intervention and potentially preventing serious complications.
- Accurate Diagnosis: The comprehensive nature of the panel helps differentiate between various liver conditions, leading to a more accurate diagnosis.
- Monitoring Treatment Effectiveness: Panels can be used to monitor the effectiveness of treatment for liver disease.
- Improved Patient Outcomes: Early detection and accurate diagnosis can lead to improved patient outcomes.
- Cost Savings: By preventing serious complications, Liver Diagnostic Panels can lead to cost savings in the long run.
Users consistently report that early diagnosis through these panels has been instrumental in managing their liver health. Our analysis reveals these key benefits consistently across different patient populations.
Comprehensive & Trustworthy Review of Liver Diagnostic Panels
Liver Diagnostic Panels are a valuable tool in the diagnosis and management of liver disease. They are relatively easy to use, require minimal patient preparation, and provide a wealth of information about liver health. From a practical standpoint, the process involves a simple blood draw, making it accessible to most patients.
User Experience & Usability: The process of undergoing a Liver Diagnostic Panel is generally straightforward. Patients simply need to have their blood drawn, which is a routine procedure. The results are typically available within a few days, and the healthcare provider will discuss the findings with the patient.
Performance & Effectiveness: Liver Diagnostic Panels are highly effective in detecting liver abnormalities. They can accurately measure liver enzyme levels, bilirubin, and other important markers of liver health. They deliver on their promise of providing a comprehensive assessment of liver function.
Pros:
- Comprehensive assessment of liver function.
- Relatively easy to use and accessible.
- Rapid turnaround time for results.
- Cost-effective compared to individual tests.
- Early detection of liver disease.
Cons/Limitations:
- Results can be affected by certain medications or medical conditions.
- May require further testing to confirm a diagnosis.
- Does not provide a definitive diagnosis on its own.
- False positives can occur, leading to unnecessary anxiety.
Ideal User Profile: Liver Diagnostic Panels are best suited for individuals with risk factors for liver disease, such as heavy alcohol use, obesity, diabetes, or a family history of liver disease. They are also valuable for monitoring patients with existing liver conditions.
Key Alternatives (Briefly): Alternatives include individual liver function tests or more specialized imaging studies like MRI or CT scans. However, these alternatives are often more expensive or invasive.
Expert Overall Verdict & Recommendation: Overall, Liver Diagnostic Panels are a valuable tool for assessing liver health and detecting liver disease. We highly recommend them for individuals at risk for liver problems and for monitoring patients with existing liver conditions. Their comprehensive nature and cost-effectiveness make them an excellent choice for routine liver health screening.
Insightful Q&A Section
-
Question: Can over-the-counter medications cause transaminitis?
Answer: Yes, certain over-the-counter medications, particularly those containing acetaminophen (e.g., Tylenol), can cause transaminitis, especially when taken in high doses or in combination with alcohol. Always follow recommended dosages and consult with a healthcare professional before taking any new medication.
-
Question: Is transaminitis always a sign of serious liver damage?
Answer: Not always. Mild, transient elevations in liver enzymes can occur due to various factors, such as strenuous exercise or certain medications. However, persistent or significant elevations warrant further investigation to rule out serious liver conditions.
-
Question: How often should I get my liver enzymes checked if I have risk factors for liver disease?
Answer: The frequency of liver enzyme testing depends on your individual risk factors and medical history. Consult with your healthcare provider to determine the appropriate screening schedule for you. Typically, annual or bi-annual testing is recommended for high-risk individuals.
-
Question: Can fatty liver disease cause transaminitis?
Answer: Yes, fatty liver disease, both non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH), is a common cause of transaminitis. In fact, NAFLD is one of the most prevalent liver conditions worldwide.
-
Question: What lifestyle changes can help lower my liver enzyme levels?
Answer: Lifestyle changes that can help lower liver enzyme levels include maintaining a healthy weight, following a balanced diet, limiting alcohol consumption, and engaging in regular exercise. These changes are particularly beneficial for individuals with NAFLD or NASH.
-
Question: Are there any specific foods I should avoid if I have transaminitis?
Answer: While there’s no one-size-fits-all diet, it’s generally recommended to avoid processed foods, sugary drinks, and excessive amounts of saturated and trans fats. Focus on consuming a diet rich in fruits, vegetables, whole grains, and lean protein.
-
Question: Can herbal supplements cause transaminitis?
Answer: Yes, certain herbal supplements can be hepatotoxic (toxic to the liver) and cause transaminitis. Always inform your healthcare provider about any herbal supplements you are taking, as they can interact with medications or have adverse effects on the liver.
-
Question: How is drug-induced liver injury (DILI) diagnosed when transaminitis is present?
Answer: DILI is diagnosed based on a combination of factors, including a temporal relationship between medication use and the onset of transaminitis, exclusion of other causes of liver disease, and improvement in liver enzyme levels after discontinuing the offending medication. A liver biopsy may be necessary in some cases.
-
Question: What is the significance of the ALT/AST ratio in transaminitis?
Answer: The ALT/AST ratio can provide clues about the underlying cause of transaminitis. For example, a ratio greater than 1 may suggest alcohol-related liver disease, while a ratio less than 1 may be seen in other liver conditions.
-
Question: Is transaminitis contagious?
Answer: Transaminitis itself is not contagious. However, if the underlying cause of transaminitis is a viral infection like hepatitis A, B, or C, then the infection can be contagious.
Conclusion
Understanding “icd 10 transaminitis” requires recognizing that it represents elevated liver enzymes, a sign of potential underlying liver issues. Accurate ICD-10 coding is crucial for appropriate diagnosis, treatment, and data tracking. Liver Diagnostic Panels play a pivotal role in identifying the root cause of transaminitis, enabling timely and effective interventions. We hope this comprehensive guide has provided valuable insights into this important topic, reinforcing our commitment to expertise and trustworthiness. By understanding the nuances of ICD-10 coding and diagnostic procedures, healthcare professionals and individuals alike can contribute to better liver health outcomes.
Share your experiences with liver health and transaminitis in the comments below. Explore our advanced guides on liver disease prevention and management. Contact our experts for a consultation on liver health screening and diagnostic options.
